Arushi Kumari
Roll number- 151
4th year MBBS
11/01/2022
This is an online E-log book to discuss our patient de-identified health data shared after taking his/ her guardians sign informed consent.
Here we discuss our individual patient problems through a series of inputs from available Global Online Community of experts with an aim to solve those patient clinical problem with collective current best evidence based inputs.
This E-log also reflects my patient centered online learning portfolio.
Your valuable inputs on comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competancy in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan.
A 70 year old male patient from dhamera village came to casuality with chief complaints :
-Fever since 3 days
-SOB grade 2----> 4 since 2 days
-Right LL swelling and redness since 1 days
History of presenting illness:
- Patient was apparently asymptomatic 3 days back before admission to hospital and then he developed fever which was low grade, intermittent, relieved on taking medication and not associated with chills and rigor.
- He has SOB (grade 2 which later progressed to grade 4).
- No associated orthopnea , PND , pedal edema , chest pain or palpitations.
- He applied ointment for leg pain over right foot 3 days back and later he developed redness and swelling over right foot (no history of trauma or injury).
- With these complaints they went to a hospital and on presentation at the hospital his vitals were SpO2-74% on RA with BP 70/40 and decreased urine output.
All necessary investigations were done and he was treated with IV Antibiotics, IV antacids, IV nebulization, IV iontropes, IV multivitamins. He was put on CPAP. His conditions was explained and was advised for hemodialysis. But patient attendees was not willing for further investigation and wanted to refer to our hospital.
- Patient was admitted to our hospital ICU on 07/01/22 .
- No H/O vomitings , loose stool , pain abdomen, cough or cold.
Past history
Not a k/c/o Dm,HTN,CAD,asthma,TB
Personal History
Diet - mixed
Appetite - normal
Sleep - adequate
Bowel and bladder movements :- normal
No known allergies to food or drugs
Addictions - smokes 9 beedis / day
General Examination:
- Patient was examined in a well lit room and having taken his informed consent .
- Patient is conscious, coherent and cooperative. Well oriented to time, place and person.
- No sign of pallor, icterus, cyanosis, clubbing, koilonychia, lymphadenopathy, no edema .
Vitals :(at the time of examination)
Temp - 100 F
PR- 104 bpm
BP- 100/70mmHg
RR- 28 cpm
SpO2- 97% at RA
Systemic Examination:
CVS: S1 S2 heard
No thrills or murmur heard
Resp.system:- position of trachea :central Vesicular breath sound heard No wheezing or dyspnoea Decreased BAE
B/L crepts present in IAA and ISA
P/A : soft and non tender
Shape of abdomen: scaphoid
No palpable mass , hernial orifices , free fluid
- No signs of organomegaly
CNS examination :-
State of consciousness : conscious
Speech : normal
No signs of meningeal irritation
Cranial nerves : intact
Sensory system :-
Pain - Normal
Touch: fine touch - normal
crude touch - normal
Temp.- normal
Vibration - normal
Joint position - normal
Motor system -. Right Left
Bulk : normal normal
(on inspection and palpation)
Power :
Neck Good Good
Upper limb 5/5 5/5
Lower limb 3/5. 3/5
(on admission)
Trunk muscles Good Good
Tone :
Upper limb normal normal
Lower limb normal normal
Reflexes :-
Biceps + +
Triceps + +
Supinator + +
Knee + +
Ankle + +
Flexor Plantar Plantar
Finger nose in coordination - no
Heel knee in coordination - no
Clinical Images:
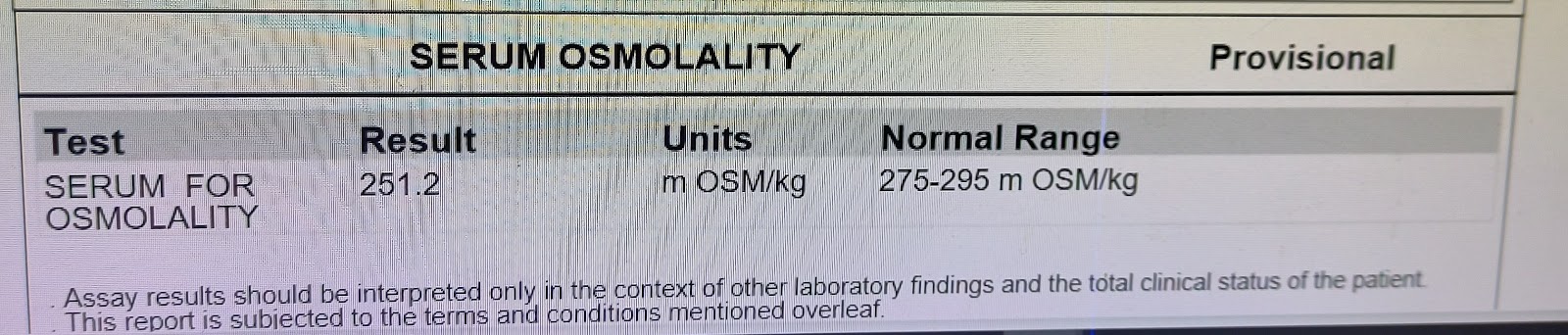
INVESTIGATIONS:
ECG
Day 1 :
2D- echo report :
ABG at 6:00 a.m
Diagnosis:
Sepsis secondary to right lower limb cellulitis
?Moderate ARDS (PaO2/FiO2= 100)
Pre renal AKI and ? Ischemic hepatitis
? Lumbar spondylosis (L2 to L5).
Treatment:
1. Propped up posture
2. O2 inhalation at 8 to 10 L/min
Maintain spO2 > 90%
3. BIPAP 4th hourly
4. Inj. PIPTAZ 4.5g /IV /stat to 2.25g IV QID
5. INJ. CLINDAMYCIN 600MG IV TID
6. INJ. PAN 40MG IV OD
7. INJ. ZOFER 4MG IV BD
8. INJ. PCM 1G IV SOS
9. T. PCM 650MG PO TID
10. IVF NS and RL at U.O + 50 ml/hr
11. INJ. NORADRENALINE at 8 ml/hr to increase or decrease acc to MAP > 65 mmhg
12. INJ. LASIX 20MG PO OD by
Update: day 2 ( 8/01/2022 )
Post debridememt right Lower limb
Patient was intubated I/v/o type 1 respiratory failiure and Respiratory distress
Drugs used -
Post intubation:
Abg:

Day 3
S: NO fever spikes
O: pt intubated and is on mechanical ventilator
ACMVPC mode
Peep 7
Fio2 100
I:E 1:2
Pt is still on ionotropes noradrenaline @16ml/hr
Vasopressin @1.5ml/hr
Pt sedated and paralysed, on dexmedetomidine 10ml/hr
Atracurium 5ml/hr
intermittent regaining of consciousnes
B/L pupil reacting to light
Vitals
Bp : 100/70mmhg
PR : 82 bpm
Spo2 : 100% on fio2 100
Grbs:121
Systemic Examination
Cvs : s1s2+
Rs: b/L basal crepts +
P/A : soft,bs+
ECG
CXR :
Treatment:
Rt feeds 200ml milk +free water 2nd hourly
IV fluids @75ml/hr
1. Propped up posture
2. O2 inhalation at 8 to 10 L/min
Maintain spO2 > 90%
3. BIPAP 4th hourly
4. Inj. PIPTAZ 4.5g /IV /stat
To inj. PIPTAZ 2.25g IV QID
5. INJ. CLINDAMYCIN 600MG IV TID
6. INJ. PAN 40MG IV OD
7. INJ. ZOFER 4MG IV BD
8. INJ. PCM 1G IV SOS
9. T. Paracetomol 650MG PO TID
10. IVF NS and RL at U.O + 50 ml/hr
11. INJ. NORADRENALINE at 8 ml/hr to increase or decrease acc to MAP > 65 MMHG
12. INJ. LASIX 20MG PO OD
On 10/01/22
S :fever spike observed
O: pt intubated and is on mechanical ventilator
ACMV pC mode
Peep 7
Fio2 60%
I:E =1:2
Pt is still on ionotropes noradrenaline @16ml/hr
Vasopressin @1.5ml/hr
Vitals:
Bp : 110/70mmhg
PR : 102 bpm
Spo2 : 100% on fio2 60%
Rr :14/min
Systemic Examination :
Cvs : s1s2+
Rs: b/L basal crepts +
P/A : soft,bs+
Rt feeds 200ml milk +free water 2nd hourly
IV fluids @75ml/hr
1. Propped up posture
2. O2 inhalation at 8 to 10 L/min
Maintain spO2 > 90%
3. BIPAP 4th hourly
4. Inj. PIPTAZ 4.5g /IV /stat
To inj. PIPTAZ 2.25g IV QID
5. INJ. CLINDAMYCIN 600MG IV TID
6. INJ. PAN 40MG IV OD
7. INJ. ZOFER 4MG IV BD
8. INJ. PCM 1G IV SOS
9. T. Paracetomol 650MG PO TID
10. IVF NS and RL at U.O + 50 ml/hr
11. INJ. NORADRENALINE at 8 ml/hr to increase or decrease acc to MAP > 65 MMHG
12. INJ. LASIX 20MG PO OD
Update :11/1/2022
S: fever spikes+
passed stools
O: pt intubated and is on mechanical ventilator SIMV PC mode
Peep 7
Fio2 45
I:E 1:2.4
RR 16
Pt is still on ionotropes noradrenaline @9ml/hr
Vasopressin @1.4ml/hr
intermittent regaining of consciousness
taking spontaneous breaths
B/L pupil reacting to light
Bp : 100/70mmhg
PR : 72 bpm
Spo2 : 100% on fio2 40
Grbs:152
Cvs : s1s2+
Rs: b/L basal crepts +
P/A : soft,bs+
A:Diagnosis:
Sepsis secondary to right lower limb cellulitis with MODS
? Moderate ARDS (PaO2/FiO2= 100)
? Acute PE
Pre renal AKI and ? Ischemic hepatitis
? Lumbar spondylosis (L2 to L5).
Treatment:
Rt feeds 200ml milk +free water 2nd hourly
IV fluids @75ml/hr
1. Propped up posture
2. O2 inhalation at 8 to 10 L/min
Maintain spO2 > 90%
3. BIPAP 4th hourly
4. Inj. PIPTAZ 4.5g /IV /stat
to inj. PIPTAZ 2.25g IV QID
5. INJ. CLINDAMYCIN 600MG IV TID
6. INJ. PAN 40MG IV OD
7. INJ. ZOFER 4MG IV BD
8. INJ. PCM 1G IV SOS
9. T. PCM 650MG PO TID
10. IVF NS and RL at U.O + 50 ml/hr
11. INJ. NORADRENALINE at 8 ml/hr to increase or decrease acc to MAP more than 65mmHg
12. INJ. LASIX 20MG PO OD






































Comments
Post a Comment