53 Year old male with SOB
Arushi Kumari
Roll no. 15
Chief complaints:
A 53 year old male ,labourer by occupation came with complaints of shortness of breath since 1 day and cough since 1 day
HOPI:
Patient was assymptomatic 2 years ago and then Developed neck pain for which he visited local hospital and was diagnosed as having hypertension and using T.Telmisartan 40mg+ T.Metapropol 50mg since then,and asymptomatic 7 days ago and then developed low grade fever and associated with chills and rigors for which they took the consultation and used injections (unknown)and his fever got subsided,and after that developed generalised weakness for which he was tested and was told to be having Typhoid positive and got treatment symptomatically for 4 days and then after 4 days ,his weakness got subsided and got his investigations done and tested positive for Dengue antibody(IgG positive)and since 23/08/2022 night developed dry cough and shortness of breath at rest,and brought here for further management
Personal history:
Mixed diet
Normal Apetite
Chronic alcoholic 90ml/day ,since 20years
Chronic smoker since 20 years.
On admission:
Pt is consious and oriented
Bp:130/100mmhg
Pulse rate:120bpm
Respiratory rate:40cpm
Spo2:62% on Room air
GRBS:151mg/dL
Respiratory system:
Bilateral air entry present
Bilateral basal crepts+
Past History :
Not a known case of Diabetes, Asthma , CAD, Epilepsy
Known case of HTN sincw 2 years and was on regular medication .
Personal History :
Diet :
Appetite: normal
Sleep: adequate
Micturition : normal
Bowel: regular
Addiction: Alcoholic since 15 years ( stopped now )
Bidi sice 15 years ( now ocassionally )
Family History :
Not significant
General Examination:
Patient is conscious , coherent and cooperative .
No Pallor
No icterus
No cyanosis
No clubbing
No lymphandenopathy
No edema
Afebrile
PR: 104bpm
RR: 31cpm
BP: 130/100 mmHg
Systemic Examination :
CVS : S1S2 heard
RS: BAE+, clear
P/A: soft. non-tender
CNS: NAD
25/08/22
Plan of Care :
- IV fluid NS 10mL
Z- Inj. Monocef 1gm IV/BD
- Inj. Pan 40mg IV/OD
- Inj. Neomol 1gm IV/SOS ( if temp.more than 101F)
- Tab. Dolo 650mg TID
- Tab. Doxy 100mg PO/BD
- Nebulization with Duolin and Budecort 8th hourly
- GRBS monitoring 6th hourly
- Monotor Vitals
Provisinal Diagnosis :
Viral Pneumonia with severe ARDS
My orientation around this case:
1. What is the reason of SOB in this patient?
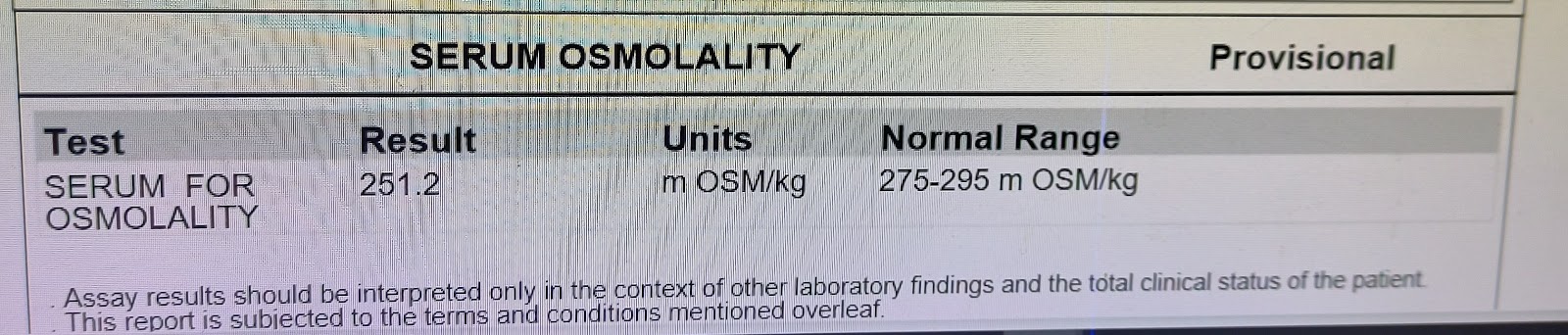
Ans. Deranged ABG
2. What is the reason of fatty liver in this patient?
Ans. Patient was chronic alcoholic



















Comments
Post a Comment