Final practical
Arushi Kumari
roll.no-151
MBBS 9th semester
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan.
45 Year old female with Rash
June 07, 2022
A 45 year old female , tailor by occupation came to the hospital with chief complain of
- On and off fever with generalized body pain since 3 months
- loss of appetite since 3 months
- itchy facial rash since 5-6 days
History of Presenting Illness
* Patient was apparently asymptomatic 10 years back when she devedoped joint pain which was gradual in onset and of fleeting type which was associated with morning stiffness which usually used to last for 10 mins and was not associated with swelling .
- Patient went to some private hospital where she was treated for the same for two months and found to be RA positive .
* Patient remained asymptomatic after being treated and since 8 months back when she developed joint pain in the metacrpophalangeal joint and knee joint following injection of 1st dose of covishield . She was treated with Inj. Diclofenac for 5-6 days and pain releived in 20 days .
* One month back patient had an episode of loss of consciousness with cold peripheries and sweating after taking Tablet Glimi M2 prescribed by the doctor for her high sugar level ( around 250 mg /dL ) .
* 10 days back patient developed fever and abdominal pain for which she was treated at a private hospital .
- Later she developed an erythematous rash over the face which was associated with itching ( increased on sun exposure)
Lesion was describe as diffuse erythematous and hyperpigmented papules ans pustules were noted over the bilateral cheeck sparing the nasolabial fold . ( Drug rash ? )
* Swelling of the left leg over the lateral aspect with erythema and local rise of temperature (? Cellulitis )
- loss of weight since 2 months
Past History :
* Patient had a history of diminution of vision at age of 15 years started using spectacles but there was gradual, progressive, painless loss of vision was diagnosed as Optic atrophy with macular degeneration .
- Not a known case of DM , asthma , TB , COPD , epilepsy .
- No relevant drug, trauma history present.
- No similar complaint in the past
Personal History :
Diet- mixed
Appetite- decreased
Bowel and bladder- regular
Sleep- disturbed
Addictions- nil
Familar History :
Patient's sister had a similar history of joint pain in the past .
General Examination :
Patient is examined in a well lit room with adequate exposure, after taking the consent of the patient.
she is conscious, coherent and cooperative, thinely built and nourished.
Pallor +
no icterus
No cyanosis
No clubbing
no lymphadenopathy
No edema.
VITALS:
Patient was afebrile at the time of presentation .
BP: 110/70bmmHg ,B/L
PR: 72bpm , regular and normal volume,felt bilaterally
RR:18 cpm
SpO2 : 98 with RA
LOCAL EXAMINATION:
left lower limb swelling was present at ankle associated with redness and local rise of temperature and dorsalis pedis pulses were felt.
SYSTEMIC EXAMINATION
CVS
Inspection:
no scars on the chest
no features of raised JVP no additional visible pulsations seen
Palpation
all inspectory findings are confirmed
apex beat normal at 5th ics
no additional palpable pulsations or murmurs
percussion showed normal heart borders
auscultation S1 S2 heard no murmurs or additional sounds
CNS: C/C/C
MOTOR-: normal tone and power
reflexes: RT LT
BICEPS ++ ++
TRICEPS ++ ++
SUPINATOR ++ ++
KNEE ++ ++
SENSORY :
touch, pressure, vibration, and proprioception are normal in all limbs
GIT:
inspection- normal scaphoid abdomen with no pulsations and scars
palpation - inspectory findings are confirmed
no organomegaly, non tender and soft
percussion- normal resonant note present, liver border normal
auscultation-normal abdominal sounds heard, no bruit present
RESPIRATORY:
inspection: normal chest shape bilaterally symmetrical, mediastinum central
no scars, Rr normal, no pulsations
palpation: Inspectory findings are confirmed
percussion: normal resonant note present bilaterally
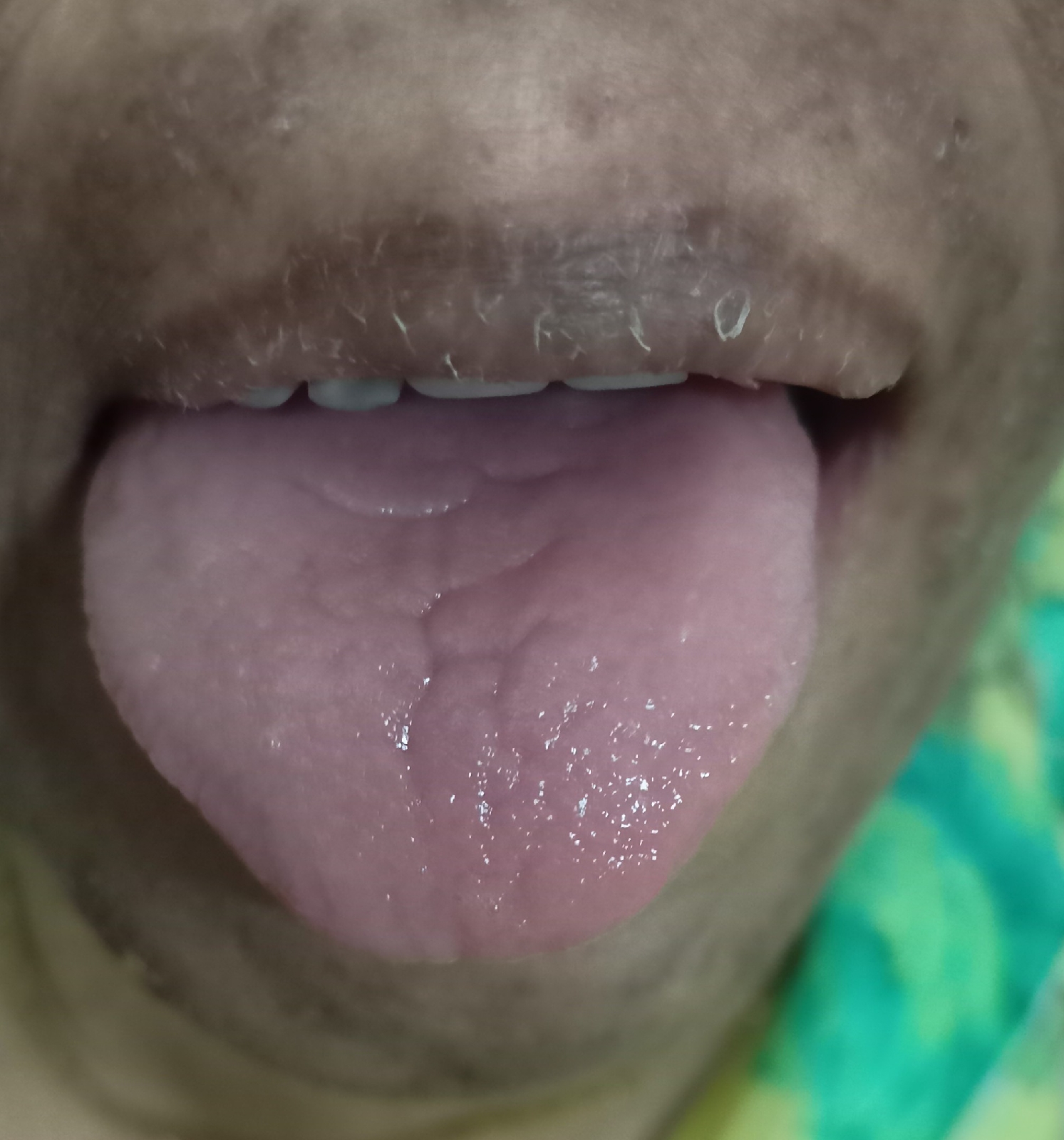
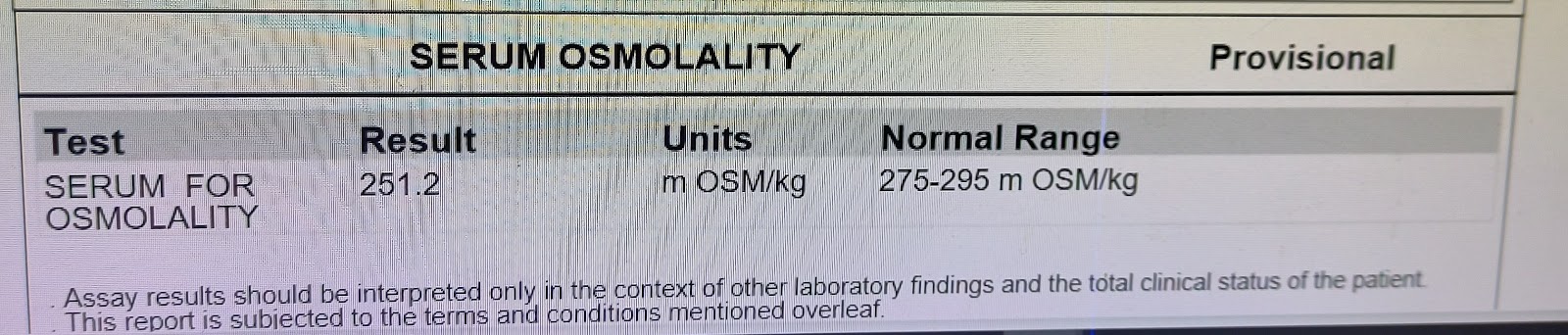
Related Images
Plain rasiograph of hand
X-ray chest PA view Reports :
US abdomen
US scan of whole abdomen
Raised RA factor
Raised SGPT and SGOT
Special tests
Impression :
Normocytic hypochromic ( Hb 6.0 )
Mild decrease in Platelet count
Overall Investigations :
RBS: 136mg/dl
HEMOGRAM:
HB: 6.9
TC: 9700
MCV: 85.1
PCV: 21.7
MCH: 27.1
MCHC: 31.8
PLT: 1.57
ESR: 90
SMEAR: ANISOCYTOSIS
RFT:
Blood Urea: 20mg/dl
S. Creatinine: 1.1mg/dl
Na: 136
K: 3.3
Cl: 98
LFT:
TB: 0.45
DB: 0.17
AST: 60
ALT: 17
ALP: 138
TP: 6.3
ALB: 2.18
CUE:
ALB +
Sugars nil
Pus cells nil
ESR - 90
CRP - NEGETIVE
HCV: NEGETIVE
HBV: NEGETIVE
HIV: NEGETIVE
Shirmer test : Investigation of choice
Fig : ANA report
Teeatment History
On 1st day ( 02/06/22 )
Inj. Piptaz 4.5 gm / iv / tid
Inj. Metrogyl 600 mL /iv / tid
Inj. Neonol 1 gm /iv / SOS ( if temp more than 101 F )
Tab. Chymoral forte PO/ TID
Tab Pan 40/ PO/ OD
Tab teczime 10 mg / PO/ OD
Hydrocortisone cream 1 per cent / OD face * week
Tab Orofer XT / OD
Inj. Nervz 1 amp in 100 mL NS
On day 2 ( 03/08/22 )
Inj. Piptaz 4.5 gm / iv / tid
Inj. Metrogyl 600 mL /iv / tid
Inj. Neonol 1 gm /iv / SOS ( if temp more than 101 F )
Tab. Chymoral forte PO/ TID
Tab Pan 40/ PO/ OD
Tab teczime 10 mg / PO/ OD
Hydrocortisone cream 1 per cent / OD face * week
Tab Orofer XT / OD
Inj. Nervz 1 amp in 100 mL NS
On day 5 (06/06/22 )
Tab Deflezacort 6mg / PO /BD
Tab Cefixime 200 mg / PO / BD
Tab. Orofer XT / PO / OD
Tab. Teczine 100 mg / PO/OD
Tab Rantac 150 mg / PO/OD
Hydrocortisonebcream 1 per cent OD for face * 1 week
Onlast day ( 07/07/22 )
Tab Deflezacort 6mg / PO /BD
Tab Cefixime 200 mg / PO / BD
Tab. Orofer XT / PO / OD
Tab. Teczine 100 mg / PO/OD
Tab Rantac 150 mg / PO/OD
Hydrocortisonebcream 1 per cent OD for face * 1 week
PROVISIONAL DIAGNOSIS:
? Secondary sjogren syndrome
Anaemia secondary to chronic inflammatory disease
with Left Lower limb cellulitis
B/L Optic atrophy
















Comments
Post a Comment